What is Meniere's Disease
“The only predictable thing about Meniere’s Disease is its unpredictability”
Described by French ear specialist Prosper Meniere in 1861, Meniere's Disease is a disorder of the inner ear characterized by three symptoms: attacks of dizziness, ringing in the ear, and fluctuating hearing loss.
During these attacks, patients suffering from the classic form of the illness first notice a low-pitched tinnitus, or ringing in the ear, often described as the sound of an ocean inside of a sea shell. This is followed shortly by intense dizziness and hearing loss. Patients describe the dizziness as a sensation of spinning or whirling. Generally, during an attack the patient cannot stand up without the fear of falling and is unable to walk. Often there is nausea and vomiting. The attack usually lasts from minutes to hours. The dizziness then gradually subsides and hearing returns to normal. Often the patient feels completely well by the following day.
Many patients, however, do not develop the three typical symptoms of Meniere's Disease at once, but may first suffer from attacks of either hearing loss or vertigo. These patients usually go on to develop the classic combination of symptoms months or years later.
There are rarer variations of the disease, including one during which hearing actually improves. Another variation is characterized by drop attacks, during which patients suffer such sudden, intense vertigo that they fall to the ground.
The severity, frequency, and length of Meniere's Disease attacks are extremely variable. Some people experience several episodes a day, while others have them only once every several years. Episodes may come in clusters and then disappear entirely for months or even years. The disease may then flare up again for several weeks or months and disappear again. This pattern of remission and recurrence occurs with or without treatment.
In the long run, the vertigo eventually “burns out”. This may take 10-15 years. Hearing, on the other hand, gradually deteriorates over a period of years and is eventually reduced to about 50% function. Other annoying symptoms such as a pressure in the ear or tinnitus may become constant and persistent over the years. 15 to 20 percent of patients develop the condition in both ears. However, it is unusual for these patients to develop active Meniere's in both ears at the same time.
WHAT CAUSES MENIERE’S DISEASE?
Although the exact cause of Meniere's Disease is uncertain, researchers believe that it results from an imbalance in fluid pressure within the inner ear, called hydrops. What causes this fluid imbalance is unclear, but includes many different predisposing factors such as infection, allergy, immune disorders, anatomical abnormalities, genetic abnormalities, and trauma. The attacks of dizziness are a result of a trigger, often unknown, which influences the underlying pathology of the inner ear.
How does it work? The inner ear, including the hearing and balance systems, is a complex series of bony chambers within the base of the skull. These chambers are filled with fluid and are further sub-divided by thin membranes into two compartments containing two different fluids, endolymph and perilymph. The fluid system, which is continuous between the hearing and balance systems, bathe the nerve endings of the inner ear and provide nutrients and a cleaning mechanism. The fluid is in a state of equilibrium; it is made and resorbed at exactly the same rate, maintaining a constant pressure.
When an attack is imminent, the endolymph fluid compartment begins to develop high pressure because either too much fluid is being produced or not enough is being absorbed. If the pressure becomes great enough, the fragile membranes separating the perilymph from the endolymph rupture, allowing perilymph and endolymph to mix. The mixture poisons the hearing and balance systems, and Meniere's symptoms result.
Once the fluid drains and pressure is reduced, the leak in the membrane heals. Normal fluid composition is restored and the balance and hearing functions gradually return to normal.
Much research is currently underway, as this process is not well understood. Research goals are to identify the triggers for attacks, identify predisposing conditions, to understand the processes occurring in the inner ear, and to develop reliable treatments.
DO YOU HAVE MENIERE'S DISEASE?
If your symptoms include episodes of hearing loss, tinnitus, pressure, and vertigo you may have Meniere’s disease.
However, there are several conditions which cause Meniere's like symptoms including viral infections, acoustic neuromas, Lyme’s disease, syphilis, cardiovascular disease, and head injury. There are literally hundreds of causes of dizziness. It is not a condition, but a symptom, and anyone who develops dizziness should have his or her balance system, hearing, and blood tested to identify the cause. A complete history and physical exam should be performed as well as special testing such as balance testing and a MRI scan. An otologist/neurotologist is specially trained to evaluate and treat dizziness related to the inner ear.
TREATMENT OF MENIERE'S DISEASE
The primary goal of treatment for Meniere’s disease is control of vertigo, the most disabling symptom. Maintenance and recovery of hearing is sometimes possible if treated early. Remember, that the disease waxes and wanes, and sometimes improves without treatment. This is the primary reason it has been so difficult for scientists and doctors to develop and test treatment strategies. Each patient will require a course of treatment designed specifically for him/her. The doctor will monitor the patient for symptoms and adjust the therapy as needed. A symptom diary will be very helpful to your doctor in doing this.
MEDICAL TREATMENT
There have been a variety of medical measures proposed for treating Meniere's Disease such as salt restricted diets and diuretics. Initial treatment should consist of a salt restricted diet. Salt restriction should consist of limiting dietary intake of sodium to 1200 to 1400 mg per day. The guidance of a diet book on sodium is very helpful. See our hints for a low salt diet. The addition of a diuretic (water pill) such as dyazide or hydrochlorothiazide can further improve the course of the disease.
There are medications available which can temporarily relieve the dizziness associated with Meniere's Disease. One commonly prescribed drug, meclizine (Antivert), is similar to Dramamine, a common over the counter drug taken for motion sickness. Neither drug has a true effect on the balance center of the brain, and does not stop the spinning. However, they sedate the patient and suppress nausea. A drawback to this treatment is that the pills take about 40 minutes to work, and by that time most Meniere's attacks have subsided. Some patients can sense an attack is coming, however, and can sometimes benefit from taking the medication in advance. Medications such as valium and ativan can also be used to manage severe the severe vertigo associated with the attacks.
In patients with attacks that seem to be triggered by allergy, allergy treatment can be very effective. This may include medications, allergy shots, and/or special diets. A trial of immune suppression is indicated for patients with autoimmune induced symptoms.
A relatively new approach uses a device called the Meniett. The Meniett device delivers a computer-controlled, complex algorithm of low-pressure pulses that are transmitted to the middle ear, where they act on the inner ear. It is believed that the energy of the pressure pulses causes a displacement of inner ear fluids, which relieves endolymphatic hydrops and symptoms of Ménière's Disease. This approach has given many patients relief, but has not been scientifically proven at this time.
Another relatively new approach uses steroids, either orally or by injection to the inner ear. The steroid acts to reduce inflammation and in some patients seems to provide limited relief. A number of other medication and herbal remedies have been proposed as treatments for Meniere’s disease but because of the capricious nature of the disease no true proof exists of their efficacy.
SURGICAL TREATMENT
80% of patients are able to gain adequate control of vertigo spells using medications and other non-surgical treatments. For the 20% of patients who fail, surgery is a good option.
There are four common operations for Meniere's Disease. Each is directed toward the relief of dizziness, but will not arrest progress of the disease or hearing loss in the affected ear. Each operation has different levels of benefit and risk. You and your physician will decide if surgical treatment is best for you, and if so, which operation would help most.
The first operation is called is called Endolymphatic sac surgery. The sac, into which fluid from the inner chamber of the ear drains, is exposed and opened. About two thirds of the patients who have this surgery seem to get better and the complication rate is extremely low. The risk of hearing loss is very small.
The second operation, called a vestibular nerve section, has a high success rate but is the most complex. During the procedure, the surgeon will cut the vestibular nerve, which carries the balance signal from the inner ear to the brain. The hearing nerve is exposed, but not cut, with the goal of preserving hearing. The success rate for eliminating dizzy spells using this procedure is about 95%. Because the balance nerve is cut, patients are usually quite dizzy for a period of days or weeks following surgery. Gradually, the balance system on the other side compensates and the dizziness disappears.
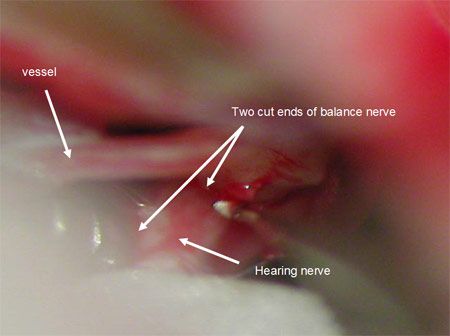
This is a picture of the balance nerve as it is cut during surgery. The balance nerve retracts when sectioned, leaving the hearing nerve exposed beneath.
The third operation to control dizziness from Meniere's Disease has a 98% success rate, but guarantees a total loss of hearing in the affected ear. The procedure is called a labyrinthectomy and is best for patients who have little or no hearing left in the affected ear. During the procedure, all of the membranes of the inner ear are removed. Like patients who have undergone vestibular nerve sections, labyrinthectomy patients are usually dizzy for a period of days or weeks until the other side and the brain compensate.
Intratympanic gentamicin therapy is an office procedure. In this procedure an antibiotic solution that is toxic to the vestibular hair cells (the balance receptor cells) is injected into the middle ear. It is an outpatient procedure and is effective in controlling the vertigo associated with Meniere’s disease. The rate of hearing loss associated with the procedure is higher than an endolymphatic sac operation but the control of vertigo appears to be better.
In summary, Meniere's Disease is a disorder of the inner ear that produces episodes of vertigo and progressive nerve deafness. A thorough examination by a qualified ear, nose, and throat specialist is needed to make the diagnosis and exclude other treatable or dangerous causes of these symptoms.
HINTS FOR PATIENTS WITH MENIERE’S DISEASE
- No smoking: Patients must abstain from tobacco totally. Nicotine is toxic to the inner ear and continued use may render all treatments listed below ineffective.
- Low sodium (low salt) diet: To decrease the amount of fluid in the inner ear, patients are placed on a low sodium diet. This means no additional salt in cooking or at the table.
- Diuretic: A diuretic is advisable to decrease the body's sodium and water content, but some diuretics decrease potassium excessively. To prevent this, patients should eat potassium-rich foods every day. Good sources of potassium are salt substitutes, orange juice, bananas, dried fruits, raisins, cantaloupe, nectarines, winter squash, navy beans, potatoes, and salt-free peanuts. Occasionally, severe weakness and "flulike" symptoms may be caused by potassium loss. It is important for patients with these symptoms to be checked promptly by a physician.
- No caffeine: Caffeine products (for example, coffee, tea, cola beverages, and chocolate) should not be used by patients with Meniere's. Numerous patients have reported attacks within minutes of caffeine use. Decaffeinated products are fine.
- Stress avoidance: Episodes of Meniere's frequently occur at times of severe stress and fatigue or immediately following such episodes. Patients should try to avoid situations that produce undue stress. At times, professional counseling is necessary to help patients with stressful problems.
- Watch for food allergy: In certain patients, episodes of Meniere's are caused by specific foods (for example, chocolate, red wine, wheat, beer, shellfish, and milk products). While this is uncommon, it is desirable to keep a list of foods ingested at the meal preceding each episode to see if any particular food is consistently present.

